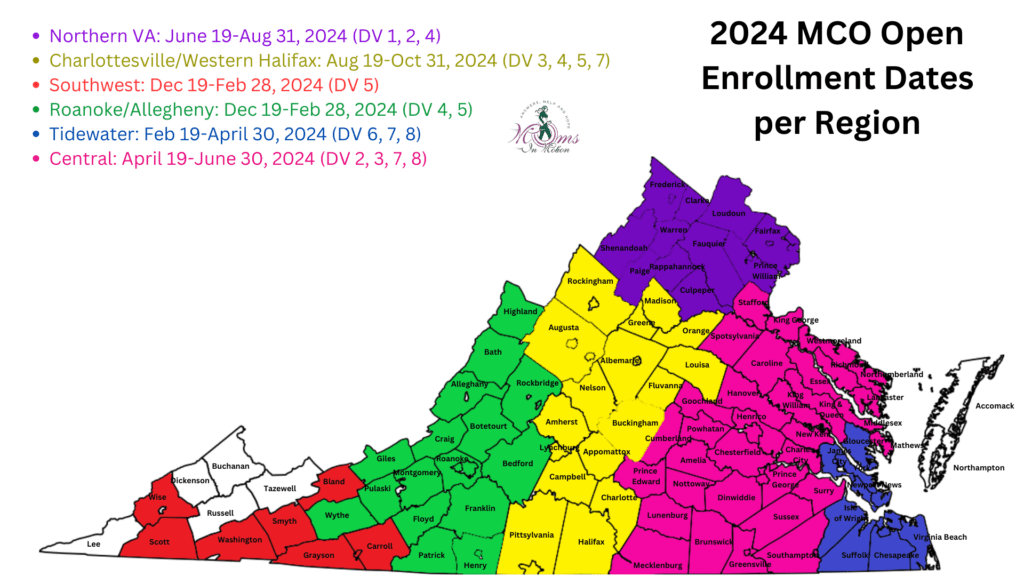
Open Enrollment
- Change their health plan for any reason.
- Review the added benefits from all health plans to see what best meets their needs.
- Call the Enrollment Helpline to ask questions: 1-844-374-9159.
When can a person change health plans?
- In the first 90 days after a person becomes a CCC Plus member
- During open enrollment
- At other times, if approved by the Department of Medical Assistance Services (DMAS)
If the person likes their current plan, they do not need to do anything.
Compare Plans
To compare plans, please click here for English and here for Spanish.
Most cities and counties in Virginia have three or four Managed Care Organizations (MCOs). These are also called health plans. Each health plan offers different services and places to get healthcare.
Basic Health Plan Benefits
- All MCOs offer these basic benefits to members:
- Behavioral (mental) health services, counseling and 24/7 crisis line
- Care Coordination services
- Durable Medical Equipment (DME) and supplies
- EPSDT services (checkups, immunizations, screenings, etc.)
- Interpreter and translation services
- No co-pays for medical services
- Person maintains obligation towards LTSS Patient Pay
- Person maintains obligation towards any Medicare Part D drug co-pays
- Physical, occupational and speech therapies and audiology services
- Prescription drugs and over-the-counter medications (when prescribed by doctors)
- Preventive and regular medical care
- Routine eye exams and glasses for children and routine eye exams for adults
- Team approach (interdisciplinary care)
- 24/7 nurse advice line
- Women’s health services
- Check the member handbook for a complete list of services.
- If the person has other insurance in addition to Medicaid, such as Medicare, the other insurance must pay first. The CCC Plus health plan will work with the person and the other insurance company to coordinate services.
Additional Benefits
- CCC Plus plans also offer added benefits such as phone services and wellness programs.
- Check the member handbook for a complete list of services.
Tips for Choosing a Health Plan
- Find out what plans are serving the person’s county and choose the best option where the person lives.
- Use these questions to help the person choose a plan:
- Does the health plan have the doctors, hospitals, and specialists the person sees?
- What additional services does the plan have?
- For questions or help selecting a health plan, please call the CCC Plus HelpLine: 1-844-374-9159 (TTY: 1-800-817-6608)
Long Term Services & Supports
- All plans cover LTSS whether the person is in the CCC Plus Waiver Program or in a nursing home. LTSS can help the person live in their own home or another location of their choice.
- LTSS includes:
- Adult Day Health Care
- Assistive TechnologyProducts, equipment, and systems that enhance learning, working, and daily living for persons with disabilities. More
- Environmental Modifications
- Nursing Institution/Hospital
- Personal Care/Respite Care
- Personal Emergency Response System (PERS)Term that refers to a device, usually wearable, that enables a person to call for help in an emergency by pushing a button. PERS devices are tagged to particular people, so the user does not need to self-identify and ask for particular supports after pushing the button for help. More
- Private Duty NursingHourly, skilled nursing care provided in a patient’s home. Private duty nursing provides more individual and continuous skilled care than can be provided in a skilled nurse visit through a home health agency.
- LTSS includes:
DD Waivers (CL/FIS)
Recipients of a Developmental Disabilities (DD) Waiver will be enrolled in CCC Plus for non-waiver services (medical coverage). The MCO will cover these benefits. DMAS will be responsible for covering waiver services, such as Personal Care, RespiteShort-term care for a child or adult that allows the primary caregiver relief. More, and CompanionA waiver-paid service focused on presence of a caregiver for safety, but less on hands on caregiving. More. Please review our CL/FIS page for a list of waiver services available to those on Virginia’s DD Waivers.
The following services are also covered by DMAS or a DMAS contractor for those on Virginia’s DD Waivers:
- Dental services through Smiles for Children.
- School health services, organized by the child’s school.
To compare the additional benefits for each plan, go to the Compare Plans section above.
Enrollment
Ready to enroll with an MCO? There are two ways in which a person can enroll in a selected MCO:
- Online (desktop or laptop)
- By Phone
- Toll-free: 1-844-374-9159
- TTY: 1-800-817-6608
To check enrollment status after enrolling, click here.
Authorized Caller Information
Speaking with the CCC Plus HelpLine for a person requires the person’s permission. If the person is a child, cannot talk, or isn’t available to give permission, the relation to the person must be stated. The following information is also required:
- The person’s Medicaid ID number
- The person’s name, address, and phone number
- The person’s Social Security Number or date of birth
Healthcare professionals also need the person’s permission to call the HelpLine on their behalf. However, public guardians and ombudsmen may speak for a person without permission.
Frequently Asked Questions
Your questions are important. The FAQ here is a good place to start to learn about CCC Plus, health plans, and PCPs. For additional questions, please call 1-844-374-9159.
Provider Search
- To see if a provider is in-network for an MCO, please complete a provider search here.
- Please contact the person’s provider to verify they are in-network. Provider search results may vary.
Please Note: A person cannot opt in and/or out from one insurance company to another unless it’s open enrollment. In special circumstances, a person can call Commonwealth Coordinated Care Helpline at 1-844-374-9159. They will make the determination as to whether or not the person’s special circumstance warrants change. Additionally, they can speak with a person in other languages.